February 2, 2022
A recent article in the Lancet Infectious Diseases presents a large scale study of post-vaccination infection conducted in the United Kingdom to assess potential long-haul symptoms. It was a
prospective, community-based, nested, case-control study that used self-reported data such as demographics, geographical location, health risk factors, COVID-19 test results, symptoms, and vaccinations) from adult (≥18 years) users of the COVID Symptom Study mobile phone app.
For the analyses, cases had received a first or second dose of a COVID-19 vaccine between Dec 8, 2020, and July 4, 2021; had either a positive COVID-19 test at least 14 days after their first vaccination (but before their second; cases 1) or a positive test at least 7 days after their second vaccination (cases 2); and had no positive test before vaccination. Also, they selected two control groups (who also had not tested positive for SARS-CoV-2 before vaccination): users reporting a negative test at least 14 days after their first vaccination but before their second (controls 1) and users reporting a negative test at least 7 days after their second vaccination (controls 2). Controls 1 and controls 2 were matched (1:1) with cases 1 and cases 2, respectively, by the date of the post-vaccination test, health-care worker status, and sex.
In the disease profile analysis, they then further sub-selected participants from cases 1 and cases 2 who had used the app for at least 14 consecutive days after testing positive for SARS-CoV-2 (cases 3 and cases 4, respectively). Their Controls 3 and controls 4 were unvaccinated participants reporting a positive SARS-CoV-2 test who had used the app for at least 14 consecutive days after the test, and they were matched (1:1) with cases 3 and 4, respectively, by the date of the positive test, health-care worker status, sex, body-mass index (BMI), and age.
They used multivariate logistic regression models (adjusted for age, BMI, and sex) to test the associations between risk factors and post-vaccination infection, and the associations of individual symptoms, overall disease duration, and disease severity with vaccination status.
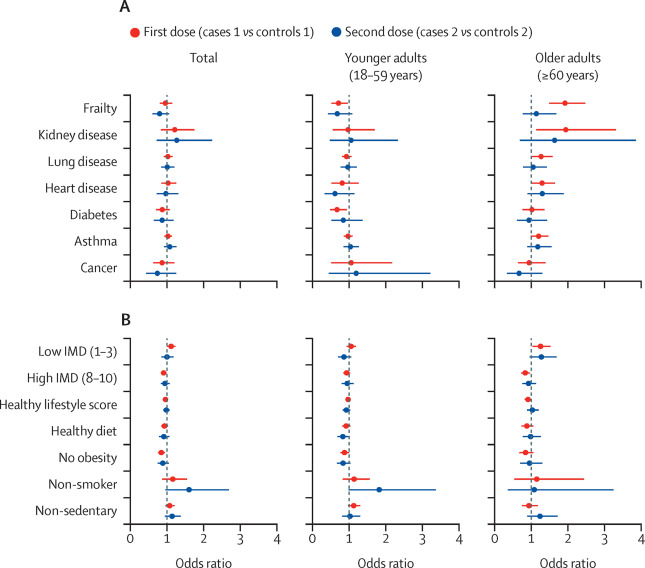
For sensitivity analyses, we examined models via inverse probability weighting31 to check for potential index event bias of vaccination using weights derived from probabilities of being vaccinated in the population tested and active on the app during the study period. The weights were estimated from a logistic regression model for predicting vaccination, including confounders known to be associated with vaccination status: frailty, IMD, and the comorbidities of cancer, diabetes, lung disease, heart disease, kidney disease, and asthma.
Between Dec 8, 2020, and July 4, 2021, COVID Symptom Study app users reported a first vaccine dose, of whom 0.5% ubsequently tested positive for SARS-CoV-2 (cases 1), and 971 504 reported a second dose, of whom 0.2% subsequently tested positive for SARS-CoV-2 (cases 2). In the risk factor analysis, frailty was associated with post-vaccination infection in older adults (≥60 years) after their first vaccine dose (odds ratio [OR] 1.93, 95% CI 1·50–2·48; p<0·0001), and individuals living in highly deprived areas had increased odds of post-vaccination infection following their first vaccine dose (OR 1.11, 95% CI 1.01–1.23; p=0·039).
Individuals without obesity (BMI <30 kg/m2) had lower odds of infection following their first vaccine dose (OR 0.84, 95% CI 0·75–0·94; p=0·0030). For the disease profile analysis, 3825 users from cases 1 were included in cases 3 and 906 users from cases 2 were included in cases 4. Vaccination (compared with no vaccination) was associated with reduced odds of hospitalisation or having more than five symptoms in the first week of illness following the first or second dose, and long-duration (≥28 days) symptoms following the second dose. Almost all symptoms were reported less frequently in infected vaccinated individuals than in infected unvaccinated individuals, and vaccinated participants were more likely to be completely asymptomatic, especially if they were 60 years or older in this study.
What was unknown in this study was if participants had prior immunity from prior infection pre-vaccination as cases. Controls could have met this criteria as well. This could have led to selection bias in their choice of cases and controls. Furthermore, perhaps the authors could have accommodated a model to allow for reinfection.
Written by,
Usha Govindarajulu
Keywords:
COVID-19, vaccination, long-haul COVID, logistic regression, biostatistics
References
Michela Antonelli, Rose S Penfold, Jordi Merino, Carole H Sudre, Erika Molteni, Sarah Berry, Liane S Canas, Mark S Graham, Kerstin Klaser, Marc Modat, Benjamin Murray, Eric Kerfoot, Liyuan Chen, Jie Deng, Marc F Österdahl, Nathan J Cheetham, David A Drew, Long H Nguyen, Joan Capdevila Pujol, Christina Hu, Somesh Selvachandran, Lorenzo Polidori, Anna May, Jonathan Wolf, Andrew T Chan, Alexander Hammers, Emma L Duncan, Tim D Spector, Sebastien Ourselin, Claire J Steves. (2022). “Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. “ The Lancet Infectious Diseases, 22(1): 43-55.
ISSN 1473-3099, https://doi.org/10.1016/S1473-3099(21)00460-6.
(https://www.sciencedirect.com/science/article/pii/S1473309921004606)